Nitric oxide modulation of respiratory motoneurons: implications for state dependent control of breathing
Obstructive sleep apnea (OSA) is one of the most common diseases in North America and it is a major risk factor for cardiovascular disease, yet neural mechanisms underlying state dependent control of respiratory motoneurons remains poorly understood. Sleep-induced loss of excitatory drive to respiratory motoneurons (i.e., disfacilitation) is well established and likely fundamental to the etiology of OSA. However, all pharmacological treatments for OSA based on this concept have been largely unsuccessful, suggesting that factors in addition to motoneuron disfacilitation contribute to OSA. We hypothesize that nitric oxide provides an inherent protective drive to respiratory motoneurons that compensates for state-dependent disfacilitation by depolarizing motoneurons through inhibition of TASK channels. We propose that disruption of this signaling pathway will contribute to OSA.
We have recently demonstrated that NO can activate respiratory motoneurons by cGMP/PKG-dependent inhibition of TASK channels and by cGMP-independent activation of HCN channels. Interestingly, NO preferentially increased the instantaneous component of the current generated by these channels by what appears to be a S-nitrosylation-dependent mechanism. Therefore, NO/cGMP and S-nitrosylation may represent new avenues for the treatment of pathological conditions resulting from loss of HMN control.
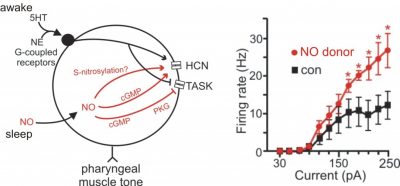
During wakefulness the HMN receives tonic 5HT, and NE drive. It is well known that these transmitters increase excitability of hypoglossal motoneurons, in part, by activation of Gq-coupled receptors and subsequent inhibition of TASK channels. The majority of this excitatory input is lost during sleep resulting in disinhibition of TASK channels, loss of motoneuron activity and narrowing of the airway. We propose that during sleep NO compensates for loss of wakeful drive by a similar mechanism involving inhibition of TASK and activation of HCN channels. Redrawn from J Neurophysiol 107:1489-99, 2012.